Overview
Urinary incontinence is the unintentional loss of urine. Stress incontinence happens when physical movement or activity — such as coughing, sneezing, running or heavy lifting — puts pressure (stress) on your bladder. Stress incontinence is not related to psychological stress.
Stress incontinence differs from urge incontinence, which is the unintentional loss of urine caused by the bladder muscle contracting, usually associated with a sense of urgency. Stress incontinence is much more common in women than men.
If you have stress incontinence, you may feel embarrassed, isolate yourself, or limit your work and social life, especially exercise and leisure activities. With treatment, you’ll likely be able to manage stress incontinence and improve your overall well-being.
Stress incontinence care at Mayo Clinic.
Symptoms
If you have stress incontinence, you may experience urine leakage when you:
- Cough
- Sneeze
- Laugh
- Stand up
- Get out of a car
- Lift something heavy
- Exercise
- Have sex
You may not experience incontinence every time you do one of these things, but any pressure-increasing activity can make you more vulnerable to unintentional urine loss, particularly when your bladder is full.
When to see a doctor
Talk to your doctor if your symptoms interfere with daily activities, such as work, hobbies and social life.
Causes
Stress incontinence occurs when the muscles and other tissues that support the bladder (pelvic floor muscles) and the muscles that regulate the release of urine (urinary sphincter) weaken.
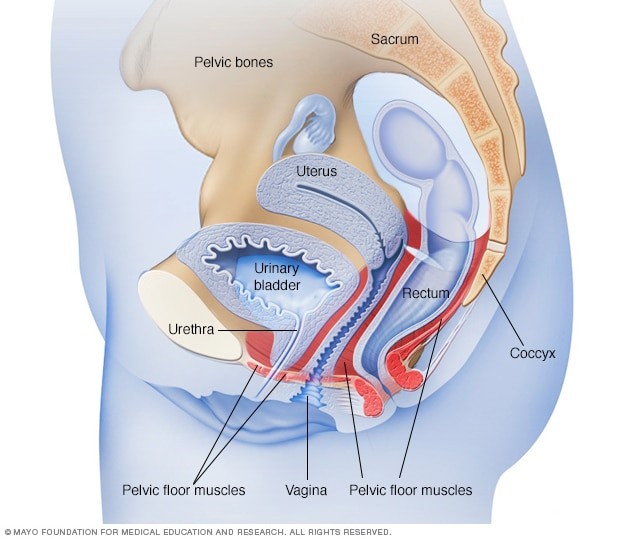
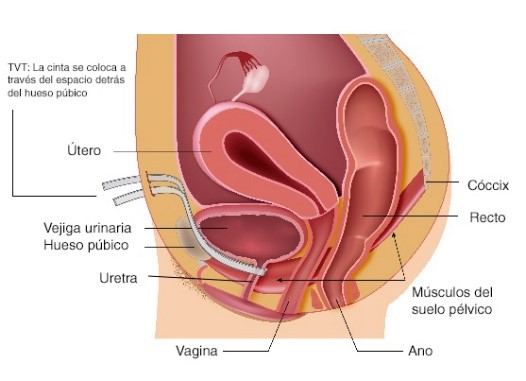
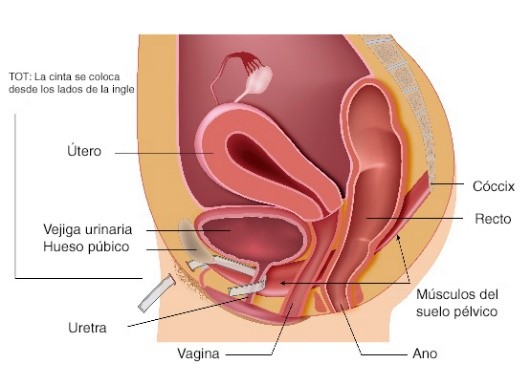
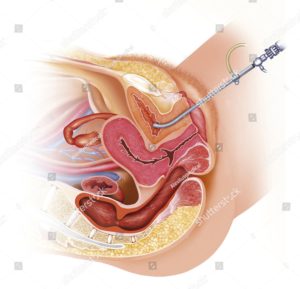
Female pelvic floor muscles
The bladder expands as it fills with urine. Normally, valve-like muscles in the urethra — the short tube that carries urine out of your body — stay closed as the bladder expands, preventing urine leakage until you reach a bathroom. But when those muscles weaken, anything that exerts force on the abdominal and pelvic muscles — sneezing, bending over, lifting, laughing hard, for instance — can put pressure on your bladder and cause urine leakage.
Your pelvic floor muscles and urinary sphincter may lose strength because of:
- Childbirth. In women, poor function of pelvic floor muscles or the sphincter may occur because of tissue or nerve damage during delivery of a child. Stress incontinence from this damage may begin soon after delivery or occur years later.
Contributing factors
Other factors that may worsen stress incontinence include:
- Illnesses that cause chronic coughing or sneezing
- Obesity
- Smoking, which can cause frequent coughing
- High-impact activities, such as running and jumping, over many years
Risk factors
Factors that increase the risk of developing stress incontinence include:
- Age. Although stress incontinence isn’t a normal part of aging, physical changes associated with aging, such as the weakening of muscles, may make you more susceptible to stress incontinence. However, occasional stress incontinence can occur at any age.
- Type of childbirth delivery. Women who’ve had a vaginal delivery are more likely to develop urinary incontinence than women who’ve delivered via a cesarean section. Women who’ve had a forceps delivery to more rapidly deliver a healthy baby may also have a greater risk of stress incontinence. Women who’ve had a vacuum-assisted delivery don’t appear to have a higher risk for stress incontinence.
- Body weight. People who are overweight or obese have a much higher risk of stress incontinence. Excess weight increases pressure on the abdominal and pelvic organs.
- Previous pelvic surgery. Hysterectomy in women and particularly surgery for prostate cancer in men can alter the function and support of the bladder and urethra, making it much more likely for a person to develop stress incontinence.
Complications
Complications of stress incontinence may include:
- Personal distress. If you experience stress incontinence with your daily activities, you may feel embarrassed and distressed by the condition. It can disrupt your work, social activities, relationships and even your sex life. Some people are embarrassed that they need pads or incontinence garments.
- Mixed urinary incontinence. Mixed incontinence is common and means that you have both stress incontinence and urge incontinence — the loss of urine resulting from an involuntary contraction of bladder muscles (overactive bladder).
- Skin rash or irritation. Skin that is constantly in contact with urine is likely to be irritated or sore and can break down. This happens with severe incontinence if you don’t take precautions, such as using moisture barriers or incontinence pads.
Diagnosis
During your visit, your doctor looks for clues that may also indicate contributing factors. Your appointment will likely include a:
- Medical history
- Physical exam with particular focus on your abdomen and genitals
- Urine sample to test for infection, traces of blood or other abnormalities
- Brief neurological exam to identify any pelvic nerve problems
- Urinary stress test, in which the doctor observes urine loss when you cough or bear down
Tests of bladder function
Your doctor might order urodynamic tests, which are used to assess the function of your bladder. Testing isn’t necessary in most cases of uncomplicated stress urinary incontinence.
Bladder function tests may include:
- Measurements of post-void residual urine. If there’s concern about your ability to empty your bladder completely, particularly if you are older, have had prior bladder surgery or have diabetes, a test of your bladder efficiency may be needed.
To measure residual urine after you have voided, a thin tube (catheter) is passed through the urethra and into your bladder. The catheter drains the remaining urine, which can then be measured. Or a specialist may use an ultrasound scan, which translates sound waves into an image of your bladder and its contents. - Measuring bladder pressures. Some people, particularly if they have had a neurologic disease of the spinal cord, will need cystometry. Cystometry measures pressure in your bladder and in the surrounding region during bladder filling.
A catheter is used to fill your bladder slowly with warm fluid. Tests of your bladder leakage will be done during the filling to check for stress incontinence. This procedure may be combined with a pressure-flow study, which tells how much pressure your bladder has to exert in order to empty completely. - Creating images of the bladder as it functions. Video urodynamics uses imaging to create pictures of your bladder as it’s filling and emptying. Warm fluid mixed with a dye that shows up on X-rays is gradually instilled in your bladder by a catheter while the images are recorded. When your bladder is full, the imaging continues as you urinate to empty your bladder.
- Cystoscopy. This is an examination of the bladder and urethra using a scope inserted into the bladder. This procedure is usually completed in the office.
Treatment
Your doctor may recommend a combination of treatment strategies to end or lessen the number of incontinence episodes. If an underlying cause or contributing factor, such as a urinary tract infection, is identified, you’ll also receive treatment for the condition.
Behavior therapies
Behavior therapies may help you eliminate or lessen episodes of stress incontinence. The treatments your doctor recommends may include:
- Pelvic floor muscle exercises. Called Kegel exercises, these movements strengthen your pelvic floor muscles and urinary sphincter. Your doctor or a physical therapist can help you learn how to do them correctly. Just like any other exercise routine, how well Kegel exercises work for you depends on whether you perform them regularly.
A technique called biofeedback can be used along with Kegel exercises to make them more effective. Biofeedback involves the use of pressure sensors or electrical stimulation to reinforce the proper muscle contractions. - Fluid consumption. Your doctor might recommend the amount and timing of fluids you consume during the day and evening. However, don’t limit what you drink so much that you become dehydrated.
Your doctor may also suggest that you avoid caffeinated and alcoholic beverages because it’s believed that in some people these dietary irritants affect your bladder function. But, new research suggests that coffee and caffeine may not increase stress incontinence. If you find that using fluid schedules and avoiding dietary irritants significantly improves leakage, you’ll have to decide whether these changes are worth the improvement in leakage. - Healthy lifestyle changes. Quitting smoking, losing excess weight or treating a chronic cough will lessen your risk of stress incontinence as well as improve your symptoms.
- Bladder training. Your doctor might recommend a schedule for toileting (bladder training) if you have mixed incontinence. More frequent voiding of the bladder may reduce the number or severity of urge incontinence episodes.
Medications
There are no approved medications to specifically treat stress incontinence in the United States. The antidepressant duloxetine (Cymbalta) is used for the treatment of stress incontinence in Europe, however.
Symptoms quickly return when the drug is stopped. Nausea is the most common side effect that makes people stop taking the medication.
Devices
Certain devices designed for women may help control stress incontinence, including:
- Vaginal pessary. A specialized urinary incontinence pessary, shaped like a ring with two bumps that sit on each side of the urethra, is fitted and put into place by your doctor or nurse. It helps support your bladder base to prevent urine leakage during activity, especially if your bladder has dropped (prolapsed).
This is a good choice if you wish to avoid surgery. A pessary will require routine removal and cleaning. Pessaries are used mostly in people who also have pelvic organ prolapse. - Urethral inserts. This small tampon-like disposable device inserted into the urethra acts as a barrier to prevent leakage. It’s usually used to prevent incontinence during a specific activity, but it may be worn throughout the day.
Urethral inserts aren’t meant to be worn 24 hours a day. Urethral inserts are generally used only for heavy activity, such as repeated lifting, running or playing tennis.
Surgery
Surgical interventions to treat stress incontinence are designed to improve closure of the sphincter or support the bladder neck. Surgical options include:
- Injectable bulking agents. Synthetic polysaccharides or gels may be injected into tissues around the upper portion of the urethra. These materials bulk the area around the urethra, improving the closing ability of the sphincter.
Because this intervention is relatively noninvasive, it may be appropriate to consider before other surgical options. However, it’s not a permanent repair. Multiple injections are required for most people. - Retropubic colposuspension. This surgical procedure — done laparoscopically or by abdominal incision — uses sutures attached either to ligaments or to bone to lift and support tissues near the bladder neck and upper portion of the urethra.
- Sling procedure. This is the most common procedure performed in women with stress urinary incontinence. In this procedure, the surgeon uses synthetic material (mesh) to create a sling or hammock that supports the urethra.