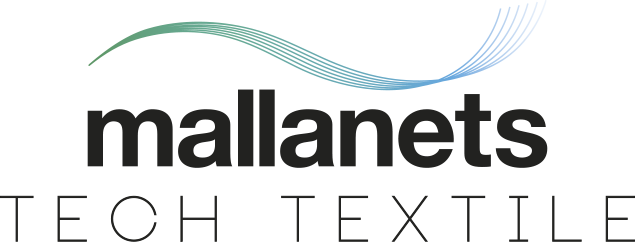
Posterior prolapse (rectocele)
A posterior vaginal wall prolapse occurs when the thin wall of tissue that separates the rectum from the vagina weakens, allowing the vaginal wall to bulge. Posterior vaginal prolapse is also called a rectocele (REK-toe-seel).
Childbirth and other processes that put pressure on pelvic tissues can lead to posterior vaginal prolapse. A small prolapse may cause no signs or symptoms.
If a posterior vaginal prolapse is large, it may create a noticeable bulge of tissue through the vaginal opening. This bulge may be uncomfortable, but it’s rarely painful.
If needed, self-care measures and other nonsurgical options are often effective. Severe posterior vaginal prolapse might require surgical repair.
Symptoms
A small posterior vaginal prolapse (rectocele) may cause no signs or symptoms.
Otherwise, you may notice:
- A soft bulge of tissue in your vagina that might protrude through the vaginal opening.
- Difficulty having a bowel movement.
- Sensation of rectal pressure or fullness.
- A feeling that the rectum has not completely emptied after a bowel movement.
- Sexual concerns, such as feeling embarrassed or sensing looseness in the tone of your vaginal tissue.
Many women with posterior vaginal prolapse also experience prolapse of other pelvic organs, such as the bladder, uterus or — for women who have had surgery to remove the uterus (hysterectomy) — the top of the vagina.
When to see a doctor
Posterior vaginal prolapse is common, even in women who haven’t had children. In fact, you may not even know you have posterior vaginal prolapse.
But sometimes moderate or severe posterior vaginal prolapses can be bothersome or uncomfortable. See your doctor if:
- You have a bothersome bulge of tissue that protrudes through your vaginal opening.
- Constipation treatment isn’t successful at producing soft and easy-to-pass stool between three times a day to three times a week.
Causes
Posterior vaginal prolapse results from pressure on the pelvic floor. Causes of increased pelvic floor pressure include:
- Chronic constipation or straining with bowel movements
- Chronic cough or bronchitis
- Repeated heavy lifting
- Being overweight or obese
Pregnancy and childbirth
The muscles, ligaments and connective tissue that support your vagina become stretched and weakened during pregnancy, labor and delivery. The more pregnancies you have, the greater your chance of developing posterior vaginal prolapse.
Women who have had only cesarean deliveries are less likely to develop posterior vaginal prolapse, but still may.
Risk factors
Factors that may increase your risk of posterior vaginal prolapse include:
- Genetics. Some women are born with weaker connective tissues in the pelvic area, making them naturally more likely to develop posterior vaginal prolapse.
- Childbirth. If you have vaginally delivered multiple children, you have a higher risk of developing posterior vaginal prolapse. If you’ve had tears in the tissue between the vaginal opening and anus (perineal tears) or incisions that extend the opening of the vagina (episiotomies) during childbirth, you may also be at higher risk.
- Aging. As you grow older, you naturally lose muscle mass, elasticity and nerve function, causing muscles to stretch or weaken.
- Obesity. Extra body weight places stress on pelvic floor tissues.
Prevention
To reduce your risk of worsening posterior vaginal prolapse, try to:
- Perform Kegel exercises regularly. These exercises can strengthen your pelvic floor muscles — especially important after you have a baby.
- Treat and prevent constipation. Drink plenty of fluids and eat high-fiber foods, such as fruits, vegetables, beans and whole-grain cereals.
- Avoid heavy lifting and lift correctly. When lifting, use your legs instead of your waist or back..
- Control coughing. Get treatment for a chronic cough or bronchitis, and don’t smoke.
Diagnosis
A diagnosis of posterior vaginal prolapse generally occurs during a pelvic exam of your vagina and rectum.
During the pelvic exam your doctor is likely to ask you:
- To bear down as if having a bowel movement. Bearing down may cause the posterior vaginal prolapse to bulge, so your doctor can assess its size and location.
- To tighten your pelvic muscles as if you’re stopping a stream of urine. This test checks the strength of your pelvic muscles.
You might fill out a questionnaire that helps your doctor assess how far the bulge extends into your vagina and how much it affects your quality of life. This information helps guide treatment decisions.
Rarely, your doctor might recommend imaging tests:
- MRI or an X-ray can determine the size of the tissue bulge.
- Defecography can determine how efficiently your rectum empties.
Treatment
Treatment depends on the severity of the posterior vaginal prolapse. Your doctor might recommend:
- Observation. If your posterior vaginal prolapse causes few or no symptoms, simple self-care measures — such as performing Kegel exercises to strengthen your pelvic muscles — may provide relief.
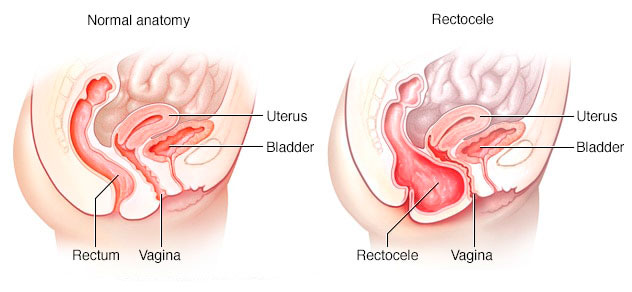
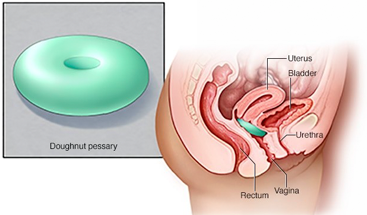
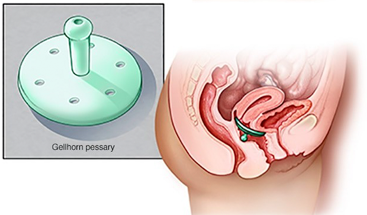
- Pessary. A vaginal pessary is a plastic or rubber ring inserted into your vagina to support the bulging tissues. A pessary must be removed regularly for cleaning.
Surgery
Surgical repair might be needed if:
- The posterior vaginal prolapse protrudes outside your vagina and is especially bothersome.
- You have prolapse of other pelvic organs in addition to posterior vaginal prolapse that is bothersome. Surgical repair for each condition can be completed at the same time.
The surgery uses a vaginal approach and usually consists of removing excess, stretched tissue that forms the posterior vaginal prolapse. A mesh patch might be inserted to support and strengthen the fascia.
Lifestyle and home remedies
Depending on the severity of your posterior vaginal prolapse, self-care measures may provide relief. Try to:
- Perform Kegel exercises to strengthen pelvic muscles and support the weakened fascia.
- Avoid constipation by eating high-fiber foods and drinking plenty of fluids.
- Avoid bearing down to move your bowels.
- Avoid heavy lifting.
- Control coughing.
- Lose weight if you’re overweight or obese.
Kegel exercises
Kegel exercises strengthen your pelvic floor muscles. A strong pelvic floor provides better support for your pelvic organs, prevents prolapse from worsening and relieves symptoms associated with posterior vaginal prolapse.
To perform Kegel exercises:
- Tighten (contract) your pelvic floor muscles as though you were trying to prevent passing gas.
- Hold the contraction for five seconds, then relax for 10 seconds. If this is too difficult, start by holding for two seconds and relaxing for five seconds.
- Work up to holding the contractions for 10 seconds at a time.
- Aim for at least three sets of 10 repetitions each day.
Kegel exercises may be most successful when they’re taught by a physical therapist and reinforced with biofeedback. Biofeedback involves using monitoring devices that help ensure you’re tightening the muscles properly for the best length of time.
Once you’ve learned the proper method, you can do Kegel exercises discreetly just about anytime, whether you’re sitting at your desk or relaxing on the couch.